Background: Elective surgical procedures are planned hemostatic challenges and laboratory coagulation testing is often the typical approach to pre-operative hemostatic assessments. This is unfortunate as the prothrombin time [PT] and activated partial thromboplastin time [aPTT] are of suboptimal predictive value for surgical bleeding risk and are have limited screening ability for inherited bleeding disorders. To the contrary, personal and family history of bleeding are important predictors of inherited bleeding disorders, and thus also likely predictive of perioperative bleeding risk. Quantitative bleeding assessment tools (BATs) have been developed to standardize the patient bleeding history, and a patient self-administered BAT (Self-BAT) has been validated for the diagnosis of type 1 von Willebrand disease. As part of a large, multicentre prospective cohort study to assess the accuracy of the Self-BAT in predicting peri-operative bleeding, we aimed to determine the correlation between results of coagulation assays and the Self-BAT score in patients undergoing elective surgery.
Methods: We enrolled adult patients with no previously identified bleeding disorder who were undergoing general elective surgery between 2017 to 2018. We excluded patients with any prior history of therapeutic dose antithrombotic use, and those undergoing cardiac, vascular, emergency, ophthalmologic, or dental surgeries. Bloodwork was drawn at the pre-operative visit, and included aPTT, PT, von Willebrand factor (VWF) antigen, VWF GP1b (ristocetin calibrated) activity, factor VIII activity, platelet function assay (PFA)-100 closure times. The pre-operative Self-BAT and all laboratory tests were analyzed at the same site . We used Spearman's correlation coefficient to determine the relationship between results of laboratory testing and the Self-BAT scores. An abnormal Self-BAT score was defined as ≥6 for women and ≥4 for men. R v4.3.1 was used to perform the analysis.
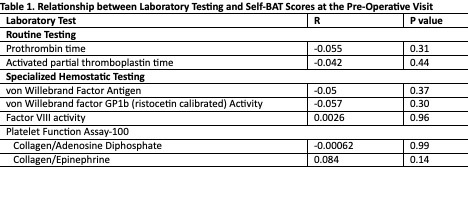
Results: A total of 368 were enrolled in the study, the mean age was 56 years old (standard deviation: 14.4) and 64.3% were women. A total of 12 individuals (3.3%) had a first degree relative with a bleeding disorder. The most common planned procedure was orthopedic (61%), followed by neurosurgery (14.4%), and general surgery (8.2%). The median Self-BAT score for women was 2 (interquartile range [IQR]: 1-4.3) and 1 (IQR: 0-2) for men. Of the 236 women and 131 men, 42 (17.8%) and 17 (13%) had abnormal Self-bat score. We found no significant correlations between the aPTT PT, Factor VIII, VWF panel nor PFA-100 and the Self-BAT score (Table 1). There was also no correlation found for sex stratified analyses.
Conclusions: Our findings confirm that unselected ‘routine’ and specialized coagulation test results do not correlate with an individual's bleeding history. Thus, indiscriminate testing should not be used as surrogate screening tests for bleeding disorders in the pre-operative setting. Specialized coagulation testing should be reserved for when a hemostatic defect is suspected based on a positive personal or family bleeding history. We look forward to the results of the primary objective of the larger cohort study; enrollment is more than half completed to determine if the Self-BAT score itself is an accurate predictor of peri-operative bleeding.
Disclosures
Teitel:Spark: Other: Clinical Trial Investigator; Octapharma: Consultancy; Biomarin: Other: participated on a Data Safety Monitoring Board/Advisory Board; Sanofi: Consultancy; Bayer: Consultancy; Pfizer: Other: Clinical Trial Investigator; Vega Therapeutics: Other: participated on a Data Safety Monitoring Board/Advisory Board. James:Star/Vega Therapeutics: Consultancy; Band/Guardian Therapeutics: Consultancy; Bayer: Research Funding. Sholzberg:Octapharma: Honoraria, Research Funding; CSL Behring: Research Funding; Pfizer: Honoraria, Research Funding.